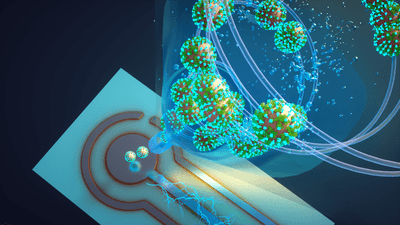
ABOVE: The air monitor acts like a tornado, trapping SARS-CoV-2 viral particles in a fluid that is sampled by a biosensor. Joseph Puthussery
Coughing, sneezing, or even talking can spread thousands of infectious SARS-CoV-2 aerosol droplets through the air.1 The COVID-19 pandemic underscored the necessity for more efficient methods to surveil indoor air quality. Recently, Rajan Chakrabarty, an aerosol scientist at Washington University in St. Louis, and his team developed a real-time monitor that detected as low as single digit viral RNA copies in the air. The study, published in Nature Communications, paves the way for improved environmental surveillance of SARS-CoV-2 in real time.2
“It was a crazy thought because of the concentrations of virus aerosols in indoor air. You [need to] be able to detect one in a million to one in a billion particles,” Chakrabarty said. “So, it's like finding a needle in a haystack.”
Achieving ultrasensitivity in detection technology was a major challenge. So, Chakrabarty recruited Joseph Puthussery, a postdoctoral researcher at Washington University in St. Louis and coauthor of the paper, to help build this machine. After many iterations, the machine was no bigger than a standard microwave and integrated two key components: a wet cyclone sampling system to capture particles and a biosensor primed to detect the SARS-CoV-2 spike protein.
Essentially, we mimic the physical appearance of a tornado in our sampling system by sucking in a high volumetric flow rate of air that creates a vortex. Then we wet the walls of the cyclone to trap the airborne particles for sampling.
– Rajan Chakrabarty, Washington University in St. Louis
First, the team determined the optimal flow rate and particle sampling efficiency of their machine using computational fluid dynamic modeling. Based on that data, they maintained a high flow rate of about 1,000 liters per minute to collect a representative sample over five minutes.
“Essentially, we mimic the physical appearance of a tornado in our sampling system by sucking in a high volumetric flow rate of air that creates a vortex,” said Chakrabarty. “Then, we wet the walls of the cyclone to trap the airborne particles for sampling.”
To detect the presence of viral particles, the fluid collected from the wet cyclone passed through the biosensor. In previous work, researchers used this biosensor to detect amyloid beta as a biomarker for Alzheimer’s disease.3 For this study, Chakrabarty’s team adapted this sensor and coated the biosensor’s electrodes with tiny antibodies, or nanobodies, derived from llamas. Llama-derived nanobodies recognized the spike protein from the SARS-CoV-2 virus and several of its variants with high efficiency.
See Also "qPCR: Driving Wastewater Surveillance for Infectious Disease"
The biosensor used voltammetry to measure the concentration of the virus. The researchers applied voltage to the sample, which oxidized the tyrosine amino acids present in the spike. Then based on the current, they determined the viral concentration. The monitor lit up if it detected live virus particles, and its high sensitivity detected as low as seven RNA copies per cubic meter of air in chamber experiments.
The integration of these two technologies is a powerful tool.
–Chang-Yu Wu, University of Miami
“The integration of these two technologies is a powerful tool,” said Chang-Yu Wu, an aerosol scientist from the University of Miami, who was not involved in the study.
Then, Chakrabarty tested the monitor’s robustness outside the laboratory. He sampled the household air of two patients who tested positive for SARS-CoV-2 by RT-qPCR. The patients were asymptomatic during the sampling period and appeared to have low virus aerosol shedding in their air samples. However, the monitor accurately identified the presence of the virus and demonstrated its high virus capture efficiency even in low-virus concentration environments.
The air monitor offers a promising solution for on-the-spot sampling and detection of viral particles for indoor applications in crowded spaces like airports and hospitals. “The building managers [could] receive important information regarding the air quality inside their building and inside different rooms at a particular time,” said Puthussery.
Moving forward, Chakrabarty and his team plan to modify the machine to capture and detect other airborne pathogens of interest.
References
- Ma J, et al. Coronavirus disease 2019 patients in earlier stages exhaled millions of severe acute respiratory syndrome coronavirus 2 per hour. Clin Infect Dis. 2021;72(10):e652-654.
- Puthussery JV, et al. Real-time environmental surveillance of SARS-CoV-2 aerosols. Nat Commun. 2023;14(3692).
- Yuede CM, et al. Rapid in vivo measurement of β-amyloid reveals biphasic clearance kinetics in an Alzheimer's mouse model. J Exp Med. 2016;213(5):677-85.